
-
 Contractual Partners
From this section it is possible to access to a description of each contractual partner of the Softis-Ped project.
Contractual Partners
From this section it is possible to access to a description of each contractual partner of the Softis-Ped project.
-
 Lecturers
From this section it is possible to access to the information about the paediatric lecturers involved in the Softis-Ped Project in the 5 European countries involved.
Lecturers
From this section it is possible to access to the information about the paediatric lecturers involved in the Softis-Ped Project in the 5 European countries involved.
-
 Residents Working with Children Information
From this section it is possible to access to the information about the paediatricians involved in the Softis-Ped Project in the 5 European countries involved.
Residents Working with Children Information
From this section it is possible to access to the information about the paediatricians involved in the Softis-Ped Project in the 5 European countries involved.
-
 Paediatric students
From this section it is possible to access to the information about the paediatric students involved in the Softis-Ped Project in the 5 European countries involved.
Paediatric students
From this section it is possible to access to the information about the paediatric students involved in the Softis-Ped Project in the 5 European countries involved.
-
 Associated Partners
As a result of the exploitation activity a number of associated partners officially joined the project in order to contribute to the improvement of the project impact on their target groups and to ensure the project sustainability by continuing using the project deliverables in the next years.
Associated Partners
As a result of the exploitation activity a number of associated partners officially joined the project in order to contribute to the improvement of the project impact on their target groups and to ensure the project sustainability by continuing using the project deliverables in the next years.
Events
The Softis-Ped project has been promoted trough conferences and articles.
-
 Conferences
The Softis-Ped project was presented in a number of events in order to report about the activities carried out and the results achieved
Conferences
The Softis-Ped project was presented in a number of events in order to report about the activities carried out and the results achieved
-
 Training Activity
The training activity 'Soft Skills in Pediatrics' was held at the University of Medicine and Pharmacy of Tirgu Mures (RO)
Training Activity
The training activity 'Soft Skills in Pediatrics' was held at the University of Medicine and Pharmacy of Tirgu Mures (RO)
-
 Press Review
The Softis-Ped project partnership made contacts with web sites focusing on the fields of paediatrics and education
Press Review
The Softis-Ped project partnership made contacts with web sites focusing on the fields of paediatrics and education
This section of the Softis-Ped portal provides administrative information for the project contractual partners and for the European Commission and it is password protected.
Training for Paediatricians and Paediatric Students
Homepage > Training > Training for Paediatricians and Paediatric Students

This training package is addressed to students and medical practitioners in paediatrics on how to autonomously learn, develop and consolidate their soft skills for improving the quality of paediatric services.
Communicating with Health Care Staff
In today’s health care system, delivery processes involve numerous interfaces among several health care practitioners with varying levels of educational and occupational training. Effective clinical practice thus involves many instances where critical information must be accurately communicated.
When health care professionals are not communicating effectively each other, patient safety is at risk for several reasons: deficiency of critical information, misinterpretation of information, unclear orders over the telephone, and overlooked changes in status. Lack of communication creates situations where medical errors can occur. On the other hand, effective communication inside health care staff can lead to positive outcomes: improved information flow, more effective interventions, improved safety, enhanced employee morale, increased patient and family satisfaction, and decreased lengths of stay.
Direct communication among health care staff encourages helpful teamwork and promotes continuity and clarity within the patient care team. However, doctors and nurses communicate differently. Nurses are focused on the “big picture” with broad and narrative descriptions of the situation, whereas doctors are focused on bullets of critical information. Good patient care is enhanced when there is mutual respect and clear communication between all health care professionals involved in the patient’s care process.
So that good clinical practice, through direct communication, involves communicating clearly, effectively, respectfully and promptly with other health care professionals caring for the patient and acknowledging, respecting the contribution of all other carers involved in the care process. Communicating sufficient information about the patient and the treatment, continuing care of patient is assured and improved especially when there is an understanding of the responsibilities, capacities, constraints and ethical codes of each other’s professions.
A large body of literature shows that because of the complexity of medical care, coupled with the inherent limitations of human performance, it is critically important that health care professionals have standardized communication tools and create an environment in which individuals can speak up and express concerns. This literature concurs that when a team needs to communicate complex information, particularly in a short period of time, it is helpful to use structured communication techniques to ensure accuracy.
A technique that seeks to bridge the gap between the different communication styles of nurses and physician is the Situation, Background, Assessment, Recommendation (SBAR) briefing model that is being used successfully to enhance handoff communication. The concept of a handoff is complex and includes communication between the change of shift, communication between care providers about patient care, handoff, records, and information tools to assist in communication between care providers about patient care. The handoff is also a mechanism for transferring information, primary responsibility, and authority from one or a set of caregivers, to oncoming staff.
SBAR consists of standardised prompt questions in four sections to ensure that staff is sharing concise and focused information. Using SBAR prompts staff to formulate information with the right level of detail.
SBAR helps to provide a structure for an interaction that helps both the giver of the information and the receiver of it. It helps the giver by ensuring she/he has formulated her/his thinking before trying to communicate it to someone else.
The receiver knows what to expect and it helps to ensure the giver of information is not interrupted by the receiver with questions that will be answered later in the conversation. SBAR can be used in any setting but can be particularly effective in reducing the barrier to effective, direct communication. It can be used anywhere, including: • inpatient or outpatient, • urgent or non urgent communications, • conversations between clinicians, either in person or over the phone - particularly useful in nurse to doctor communications and also helpful in doctor to doctor communication, • conversations with peers – change of shift report, • communication between different disciplines, • increasing a concern, • when patients move between services or from social care (care homes and into/out of hospital).
In order to achieve continuity of care it is essential that healthcare staff have the knowledge and skills to work collaboratively with others involved in the current or future care of the child and family. This involves effective communication, sharing of relevant information and supporting effective transition between services during admission or discharge from hospital.
In the inpatient setting, healthcare staff can assist in the provision and modelling of useful communication with children and their families but the practice of depending on numerous caregivers to communicate poses a risk of families being exposed to be in conflict with information and opinions, often provoking anxiety and confusion. So that, true interdisciplinary teamwork and collaboration can prevent this complication.
Communication skills such as active listening, paraphrasing, summarising, reflecting and questioning are fundamental to the development of relationships. All these relationships influence the ability to provide high quality care which is synchronized around the needs and wishes of the pediatric patient/ family, in order that they should consent and be actively involved in care decisions resulting in an agreed understanding between all stakeholders.
The health outcomes of children are affected when their caregivers struggle with health literacy; these caregivers are more likely to inappropriately dose medications by using spoons, cups and other nonstandard dosing instruments. Thus, the healthcare provider would use communication techniques that facilitate comprehension, such as teach back, for all patients/families not just those the provider perceives as being challenged with comprehension.
Teach back technique in care provider instruction is an evidence-based action where the healthcare provider first teaches a health-related topic followed by asking the patient/family to teach back, demonstrate or repeat back the information taught, repeating the cycle as necessary until understanding of the topic is accomplished. Teach back puts the burden of effective communication on the provider, by requiring the provider to explain to the patient/family information they need to apply in a manner that the patient/family understand. Patient/family understanding is confirmed when they accurately explain the information back to the provider in their own words.
Teach back is shown to improve communication, comprehension and outcomes: its elements are to assure accurate medication reconciliation at discharge and to arrange follow-up appointments before discharge, documenting the appointment day and time on the after visit summary note; it is an approach for care providers and caregivers to share meaning in the moment so that the family reproduces at home what they learned at the hospital.
The teaching-learning process of family care involves explanation, observation, execution, supervision, collaboration and performance assessment. Teaching based on demonstration and feedback appears to be central to this educational process that mediates learning of procedural care.
During the hospital discharge it is crucial that nurses take on the role of discharge coordinators, involving themselves in this transition process and integrating other team members in a group action, offering families support for daily living and building together the means to facilitate the performance of care with autonomy, safety and quality for their children at their homes.
Checkpoint on best practice – Handoff Communication and SBAR
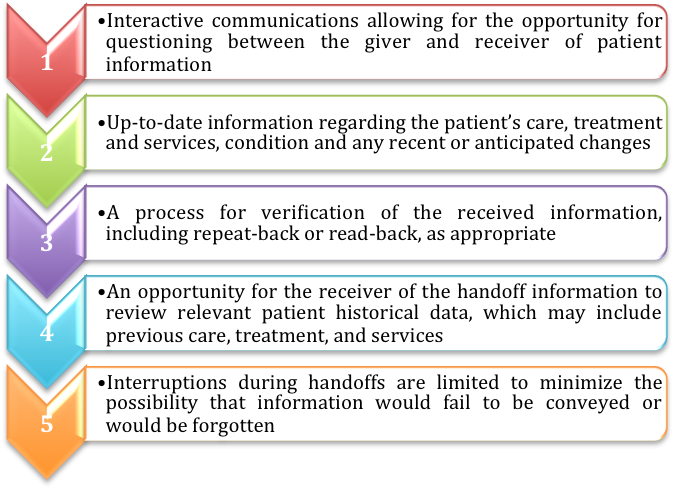 Source: Adapted from Joint Commission, National Patient Safety Goals Hospital Program
Source: Adapted from Joint Commission, National Patient Safety Goals Hospital Program
Table 1. Joint Commission 2008 Hospital Patient Safety Goals Implementation Expectations for Handoffs
- Use clear language and avoid use of abbreviations or terms that can be misinterpreted
- Use effective communication techniques. Limit interruptions. Implement and utilize read-backs or check-back techniques.
- Standardize reporting shift-to-shift and unit-to-unit.
- Assure smooth handoffs between settings
- Use technology to enhance communication. Electronic records can support the timely and efficient transmission of patient information.
Table 2. Strategies to Improve Handoff Communication
- Situation – What is going on with the patient?
- Background – What is the clinical background or context?
- Assessment – What do I think the problem is?
- Recommendation – What would I do to correct it?
Kaiser Permanente, SBAR (Situation, Background, Assessment, Recommendation) Tool, 2002
Source: Institute for Healthcare Improvement. Guidelines for communicating with physicians using the SBAR process.
http://www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm.
Table 3. SBAR – A technique for communicating critical information that requires immediate attention and action concerning a patient’s condition
| OFF GOING NURSE (complete pre shift-change activities) | |
| S Situation |
|
| B Background |
|
| A Assessment |
|
| R Recommendation |
|
| T Thank |
|
| ONCOMING NURSE | |
| S Set aside assumptions |
|
| B Be attentive |
|
| A Ask questions |
|
| R Be Responsive |
|
| T Thank |
|
Table 4. SBAR - T Format – BEDSIDE SHIFT REPORT
Checkpoint ... on best practice – Techniques of Communication and Teach Back
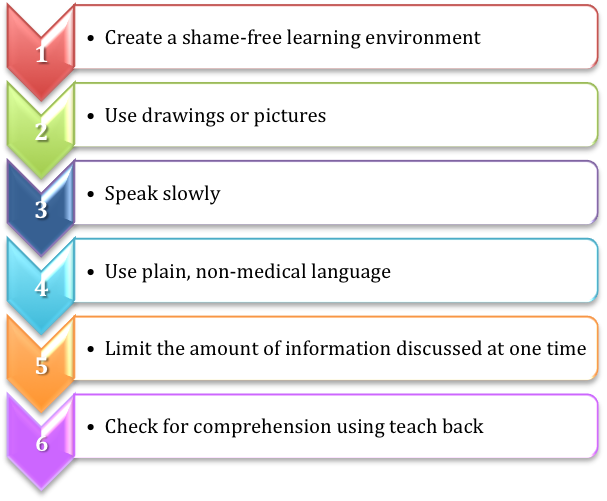 Source: Freely adapted from “Health Literacy and Teach Back for Effective Health Care Communication”
Source: Freely adapted from “Health Literacy and Teach Back for Effective Health Care Communication”
Table 5. Techniques to Improve Communication Skills
The transcript in English is available
Reflecting on professional practice:
Self-evaluation tool to check the communication tools in the video
- “Cloud” Case Study: “George is coming back home”It’s time for George to come back home
- Information booklet: how to create itNurses offering oral and written information upon admission and discharge from hospital to a pediatric patient / family.
- Example of an information bookletCentral venous catheter management for care givers at home
- Handoffs: Transitions of Care for Children in the Emergency Department This document describes transitions of care, also referred to as handoffs or sign-outs, that occur when the responsibility for a patient’s care transfers from one health care provider to another. Recommendations for development, education, and implementation of transition models are included.
- Characterizing the structure and content of nurse handoffs: a sequential conversational analysis approachThis document presents a methodological framework (SCA – Sequential Conversational Analysis) a mixed method approach, methodological approaches for studying nurse handoff communication and a case study about evaluation of nurse handoff communication.
- Handoffs: implication for nursesChapter 34 of the book presents an handoffs overview, a summary of selected literature, gaps in the knowledge and suggestions for quality improvement initiatives and recommendations for future research.
- Communicating With Children and Families: From Everyday Interactions to Skill in Conveying Distressing InformationThis article provides a review of the evidence regarding clinical communication in the pediatric setting, covering the spectrum from outpatient primary care consultation to death notification, and provides practical suggestions to improve communication with patients and families, enabling more effective, efficient, and empathic pediatric health care.
- Developing effective therapeutic relationships with children, young people and their families The aim of this article is to assist the reader to conduct a critical review of the therapeutic relationship between the children’s nurse, child and family, identifying areas for practice development. Therapeutic relationships can be defined in a variety of ways and compose differing components.
- Discourses on discharge care for children with special healthcare needsThis research analyze the discourse of healthcare professionals and families on the continuous and complex care for children with special healthcare needs; understand hospital discharge as a process centered on children demands and family learning.
- Family Centered Pediatric Nursing Care: State of the Science
(J Pediatr Nurs. 2010 October ; 25(5): 335–343. doi:10.1016/j.pedn.2009.01.006) This article illustrates the sample of 30 papers reviewed in three sections: researcher observations of parent nurse interactions, research examining the perspective of parents or family caregivers, and research examining the perspective of health professionals. - Health Literacy and Teach Back for Effective Health Care Communication
(“Patient Care – Collaborating for Best Outcomes”, a Nationwide Children’s Hospital Publication - Volume 31, Issue 3, page 21; Summer 2016) This article explains how collaboration with patients, families and healthcare staff is essential to achieve goals and strive for best outcomes as a strategic plan outlines.


